Is It Time to Recalibrate or Reconsider the Hospital Typology?
-By Henry Chao in collaboration with Brian de Francesca
“We shape our buildings; thereafter they shape us.” – Sir Winston Churchill
Ever Rising Healthcare Spending, Recent Hospital Financial Turbulence, and Skyrocketing Hospital Construction Cost
In its name alone, the United States 2010 Patient Protection and Affordable Care Act sums up the major healthcare challenge in the US for decades. Not much has changed ten-plus years after its passing. US healthcare spending grew from $2.6 trillion (17.9% of GDP) in 2012 [1] to $4.3 trillion (18.3% of GDP) in 2021 [2]. As we enter the beginning of post-pandemic years, many hospitals are still struggling with the financial damages it caused [3]. Interestingly, while hospitals are tightening their belt, some US hospitals and healthcare institutions are also embarking on building new facilities with a price tag reaching beyond $1 billion [4]. Similar ambitious construction efforts had been in the Middle East in the last 15 years where tens of thousands of hospital beds were added. As of 2022, a projected $45B new construction spending is still in the pipeline [5]. In the UK, there are the upcoming 40 new NHS hospitals with a price tag of £24bn [6].
Do hospital constructions have to cost this much? We have known that building new hospitals is an expensive undertaking. Modern hospitals are one of the costliest structures to build in comparison to other building typologies, and likely also the costliest to maintain afterwards. Hospitals are mission-critical structures; they need to be operational after a strike or a major disaster. This leads to a set of requirements in hospital construction including superb structural strength to not just avoid collapse but maintain its operation after natural disasters. Sophisticated building service systems to assure patient safety and comfort. And in the last 20 years, hospitality-quality interior finishes provide patients with a healing environment and experience, while remain the utmost flexibility to respond to ever going changes in care knowledge and technologies, operational protocol, and patient volume fluctuations.
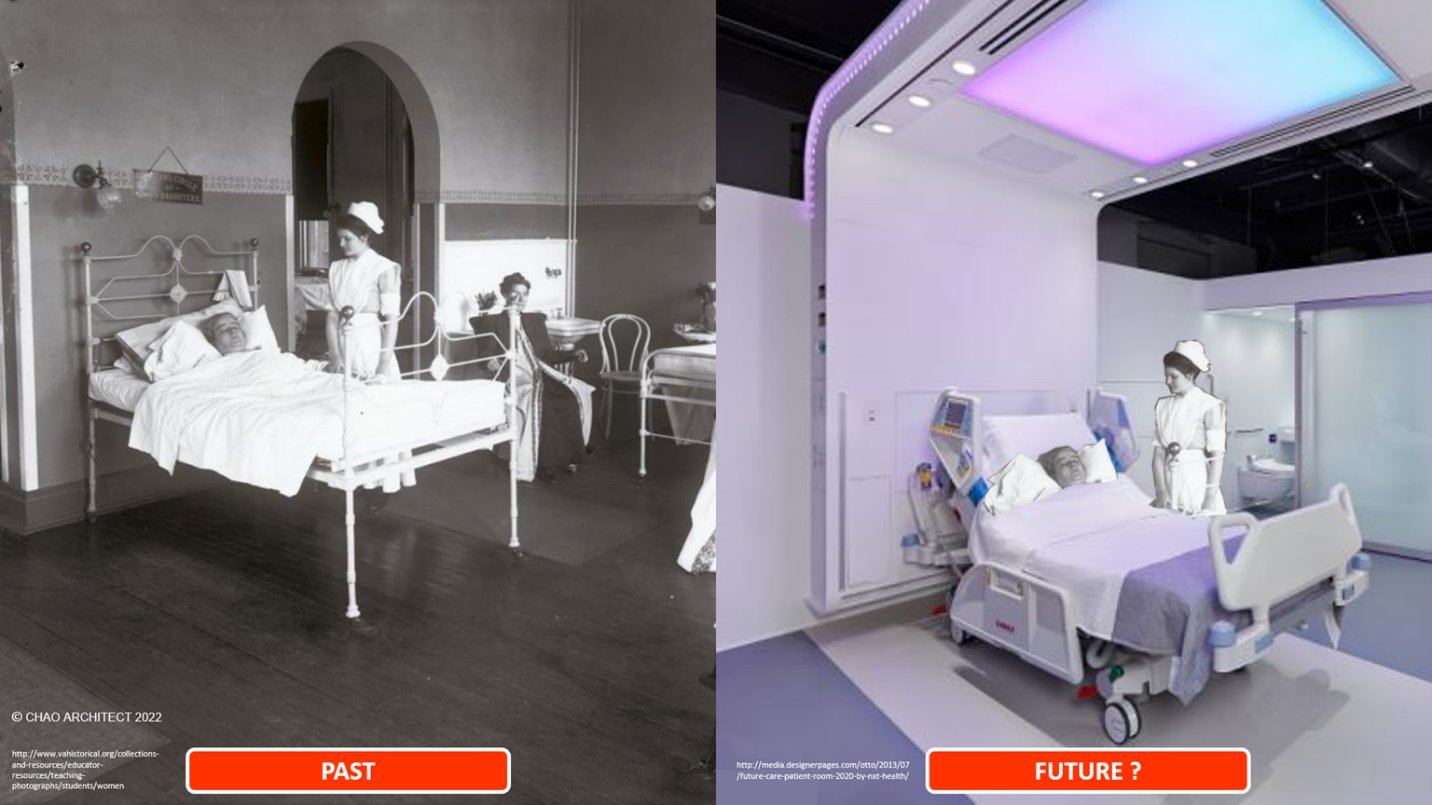
As many of the less acute medical treatment episodes migrate out of hospitals into less expensive treatment spaces, hospitals will now house patients who are sicker and demand higher protection and environmental quality from the care facilities. All these factors push the traditional hospital toward being highly sophisticated and customized healing machines that take huge amounts of financial resources and a lot of time to erect and maintain, while its own planning and design typology is based on a model that has not changed much since the Nightingale era, which might, or might not, be the correct and most effective one for the delivery of contemporary healthcare. The Covid pandemic has exposed many of its weaknesses in adequately responding to care needs.
Current Hospital Typology and Its Misalignment Contemporary Functional Needs Current hospital typology is a product of an era when the development of modern medicine coincided with the rise of the industrial revolution. The hospital structure is thought of as a machine for cure where patients are processed through stages of diagnosis, treatment, and then recovery. The facility focus for the clinical task is safety and speed, and the subsequent time and motion study and corresponding planning approach places priority on flow, adjacency, and spatial efficiency. Facility quality control is achieved through standardization and enabled best by a modular and repetitive approach. We have had MacDonald's medicine for the past century plus. However, the rise of information technology, the increase in consumer's voice, and shifting toward personalized medicine are now questioning these care protocols and, subsequently, the adequacy of the traditional hospital design model. Would a facility, which is planned and constructed for mass standardization be able to provide a mass customization care model? Comparing the current needs and what the hospital facilities are providing, I found there are four misalignments:
Misalignment #1: Design for The Worst Condition Everywhere Patients seek medical help from hospitals for all kinds of illnesses with a wide range of acuity. Traditionally, 10% of hospital beds are ICU beds. However, this model was severely tested during the Covid pandemic. As less acute patients gradually take their care to settings other than the hospital, the patients admitted into the hospital have higher acuity and are sicker, requiring elevated environmental safety from the building system during the time of care. The current planning solutions are to have either a costly setup to provide a switch on/off flexibility or equally costly, to build a higher-level building system across the entire facility. Design for the worst condition no doubt increases the hospital construction cost. Are there any other options?
Misalignment #2: Hospital Needs to Last Forever Hospital buildings are made of different systems of different materials and have different operational life span. The building structure and envelope are typically designed to last 50 years or more, as evident in many hospitals that have century-old buildings that are still operational. The mechanical system, the most crucial item for safety and comfort, has a life span of 20 to 25 years. The hospital furniture, with its 24x7 use, typically lasts about seven years. Many diagnostics and treatment equipment would likely see a new model come out every five years. On top of the physical structure is the governing information technology system which frequently has a shorter life span than its physical counterparts. So, those costly, brand-new hospital buildings really have only a few years to live up to their state of art label and will likely encounter needs of renovation and adjustment in about five years after their completion. This is the reason why you would always see some repairing or upgrading works going on in a hospital.
Misalignment #3: Size of Facility and the Business Models Once a hospital building is built, while the mission is still patient care, the business model shifts to assure those brand-new hospital beds are occupied, similar to running a hotel. The ongoing competition for patients extends the hospital operation consideration beyond just medical care excellence to include many other hospitality amenities for patients, families, and staff. There is little doubt that this race results in increases in patient satisfaction scores, but it also comes with elevated construction costs [7]. On top of that, while the capacity of the facilities is fixed, the medical demands, like a pandemic, can be fluid. The carrying cost of a large facility includes not only the utilities but also staffing, as well as other items associated with the building including impact on traffic, parking, and public safety and security. As stated by Sir. Winston Churchill, once a hospital building is built, it shapes us.
A Possible Recalibration of Care Facility? In the past two decades, many other industries have gradually drifted away from heavy facility-centric operations, but the hospital is doubling down, as described at the beginning of this article. Once built, these projects are not just for disease care, their presence also creates a significant impact on the local or regional infrastructure, traffic and parking pattern, and the real estate value of the surrounding communities. For the past decades, on small scale, hospital campuses have become economic engines for the community they reside. On a larger scale, healthcare institutions can and have become a destination, for small or medium cities. Until some kind of revolutionary change in medical care occurs, hospital building is and will continue to be a must-have component for providing health care for the foreseeable future. To adequately balance functional needs, care experience, and cost, we might need to reconsider the makeup of the current typology and explore the following ideas:
Can We leverage the System Capacity to Recalibrate How Much We Build? During the early months of the pandemic in 2020, New York City was facing a major tidal wave of Covid patients. Knowing that no one hospital or hospital system is totally ready and capable to care for the incoming patients, the government task force coordinated and distributed the patient across many participating public and private hospitals and systems while it frantically built up the overall ICU capacity. Can we continue this level of coordinated care access even not in times of pandemic so that we do not overbuild bed capacity just because of individual needs? What we need is a mechanism across different care systems that equitably distribute the patients and the care for the best clinical outcome while assure the financial health of the participating hospitals. This setup likely already exists within many hospital systems with hub and spoke operation models.
What Do We Build and How Do We Build Them? As mentioned earlier, it is likely the future hospital will house patients who are sicker and who have illnesses that are more acute. The required facility is a combination of a large emergency department, a robust diagnostic and treatment centre, and a sizable intensive care unit, all of these require more intense and higher-quality building service systems. Despite a hospital having many other support areas that do not require this level of building services, the current build-for-the-worst-scenario planning and design approach will cater the entire building system to these most stringent uses. We should carefully consider the opportunity to unbundle these services into separate building blocks and serve them with just the right amount of utility. A modularized building utility system that allows incremental adjustments for change is the most flexible and cost-effective.
A Care District In Lieu of a Mega Hospital? As care technology becomes more mobile and nimbler and the care process shifts from a departmental and stage structure to a more team-oriented and integrated approach, it might be time to consider a medical district which contains a broad range of care settings from a right-sized hospital for most intense and acute patients, to a long-term stay step-down and recovery centre, ambulatory care centre, specialists office, and rehabilitation and pharmacy, and preventative health facilities, threaded together with the physical connecting pathways and ubiquitous monitoring technology and supported by the community-based amenity businesses. This type of approach already exists in many places in an organic form, yet a planned approach can synchronize infrastructure deployment, traffic patterns, and growth and change strategy.
Gradual Transition from Project to Product Hospital constructs is made of primarily two kinds of space, areas that enable modern and sophisticated technology to perform complicated clinical interventions, and areas that are primarily for patients to have comfortable healing and recovery. The former is likely to encounter frequent changes in treatment knowledge and equipment while the latter is more grounded in long-standing community tradition. Rather than considering the hospital as just a construction project where everything is custom-made to last forever, maybe we should start considering those hi-tech spaces more like a product, with factory-made quality construction to ensure operational safety, but has a set shelf life that is synchronized with the correlated medical equipment development, situated in an architectural shell. In those hi-touch areas, it will continue to be a custom-made project to reflect the mission and value of the care institution, reflect the cultural and environmental preferences of the community it serves. The products can be and should be updated periodically to enable clinicians to practice the best clinical care. The project establishes and continues a tradition that is specific to the place and memorable.
The New Care Technologies and Alternate Places of Care Covid pandemic also provided the world with a glimpse of what digital and communication technology can do to the care process when the facility is either over capacity or just not accessible. Telemedicine, remote monitoring, mobile diagnostic technology [8], and artificial intelligence-enabled medicine to begin allowing diagnostic and even treatment activities to occur outside of the hospital campuses, into ambulatory surgical centres, medical offices, schools, and most importantly, people’s homes really should be hospital-care-able. Several studies [9] have indicated that patients who recover at home after receiving treatment in the hospital had better experiences and better clinical outcomes. CMS and several leading US medical institutions are looking into this. If this trend continues and expands, the hospital will indeed become more of a centre for emergency medicine, intervention, and intensive care beds, as well as a patient remote monitoring centre and the home base for the mobile care team, a safety net for the community via its true mission critical facility and campus.
References:
[1] https://www.cms.gov/newsroom/press-releases/growth-us-health-spending-remains-slow-2010#:~:text=The%20report%20notes%20that%20U.S.,)%20(4.2%20percent)%20rebounded
[2] https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical#:~:text=U.S.%20health%20care%20spending%20grew,spending%20accounted%20for%2018.3%20percent.
[3] https://www.beckershospitalreview.com/finance/hospitals-on-track-for-worst-financial-year-in-decades.html
[4] https://www.beckershospitalreview.com/capital/7-hospital-construction-projects-worth-1b-or-more.html
[5] https://www.zawya.com/en/press-release/events-and-conferences/mena-hospital-projects-forum-2022-to-feature-us45bln-worth-of-healthcare-projects-across-mena-region-jwmgekw9
[6] https://www.theguardian.com/politics/2019/dec/08/boris-johnson-40-new-hospitals-pledge-costed
[7] https://www.nytimes.com/interactive/2014/sunday-review/hotel-hospital-quiz.html
[8] https://health.ucdavis.edu/news/headlines/portable-mri-device-reduces-time-for-diagnosing-traumatic-brain-injuries/2022/03
[9] https://www.aha.org/hospitalathome